Corneal Transplants
Corneal transplants may be necessary when the normally clear cornea can no longer transmit or focus light properly.
The cornea is the clear, dome-shaped outermost layer of the eye that covers the iris and the pupil and plays a critical role in focusing light onto the retina. Corneal diseases are a leading cause of blindness with an estimated 10 million patients diagnosed with bilateral corneal blindness worldwide.
Corneal transplantation is typically recommended when the cornea has been damaged by injury, infection, or disease.
Typically, the transplanted corneas are from corneal tissue from a donor. Everyone is a universal donor for corneal tissue — the donor’s blood type does not have to match the blood type of the recipient. Age, eye color and eyesight are not factors either. Aside from those suffering from infections or a few highly communicable diseases, most people are potential cornea donors.
Some of the most common conditions that can be treated with a corneal transplant include:
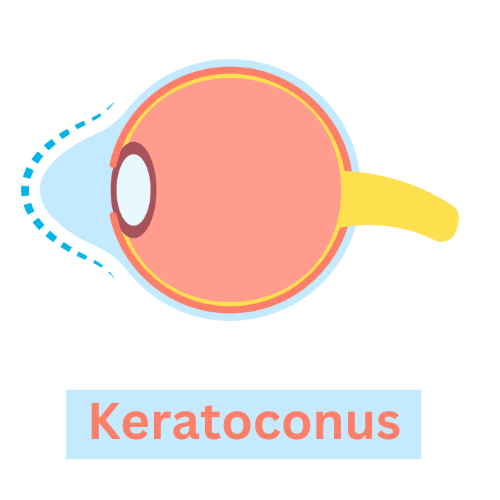
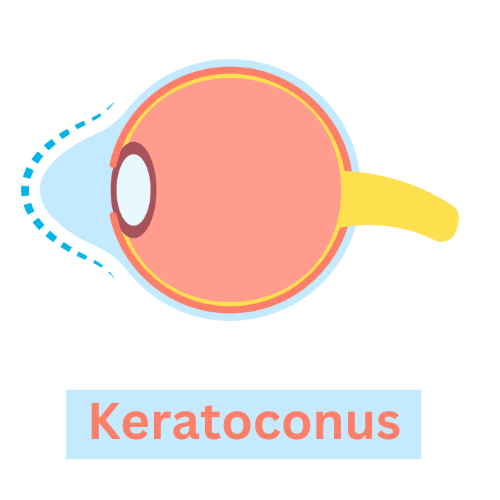
- Keratoconus: A condition in which the cornea becomes thin and cone-shaped, leading to distorted vision. See graphic above.
- Fuchs’ dystrophy: A progressive disease that affects the endothelial cells of the cornea, causing vision loss.
- Corneal scarring: Scarring of the cornea can occur due to injury or infection, leading to vision loss.
- Corneal edema: Swelling of the cornea can occur due to various factors, including disease or trauma, leading to vision loss.
- Corneal ulceration: Ulcers on the cornea can be caused by bacterial or viral infections, leading to vision loss.
- Bullous keratopathy: This condition occurs when the cornea becomes swollen and blistered, leading to vision loss.
- Corneal dystrophies: These are inherited disorders that can cause vision loss due to progressive changes in the cornea.
Types of corneal transplants
There are several types of corneal transplants, including full-thickness transplants and partial-thickness transplants, depending on the extent of the damage to the cornea.
For a full-thickness corneal transplant, the surgeon removes the entire thickness of the damaged or diseased cornea and replaces it with a donor cornea that has been carefully matched to the patient’s eye. The donor cornea is then sutured into place using very fine stitches.
This procedure is typically reserved for cases in which the damage to the cornea is severe and cannot be treated with other interventions, such as medication or less invasive surgical techniques. Full-thickness corneal transplants can be very effective in restoring vision in people with certain corneal conditions, such as corneal scarring, thinning, or clouding.
A partial thickness corneal transplant is a surgical procedure in which only a portion of the cornea is replaced with healthy donor tissue.
Partial thickness corneal transplants are typically performed in cases where the damage to the cornea is limited to specific layers and can be treated without replacing the entire cornea. They are often preferred over full-thickness transplants because they involve less tissue disruption and have a shorter recovery time. However, they may not be suitable for all types of corneal conditions, and there are still risks involved, such as infection, rejection, and astigmatism.
Recovery from a corneal transplant can take several months, and patients will need to use eye drops and take other precautions to ensure the success of the procedure.
Artificial corneas
Artificial corneas can be used to restore vision in patients who are not good candidates for a traditional corneal transplant. These devices are typically made of biocompatible materials, such as polymers or ceramics, and are designed to replace the damaged or diseased cornea.
There are several types of artificial corneas available, each with its own unique design and features. Some of these devices require the removal of the patient’s damaged cornea, while others can be implanted over the existing cornea.
Artificial corneas may be recommended for patients who have already had one or more failed corneal transplants, or for those who have a high risk of rejection due to underlying medical conditions or a history of corneal infections. However, like any surgical procedure, there are risks associated with artificial cornea implantation.
Success of corneal transplants
Corneal transplants are generally considered to be a safe and effective procedure, with a high success rate. The success of the transplant depends on various factors, such as the underlying condition and the patient’s age and health status.
According to the American Academy of Ophthalmology, the success rate of corneal transplants ranges from 80 to 90 percent. This means that most patients who undergo a corneal transplant can expect to see an improvement in their vision and an alleviation of symptoms such as pain or discomfort.
However, like any surgical procedure, there are potential risks and complications associated with corneal transplants, such as infection, rejection of the transplanted cornea, or changes in eye pressure.
Patients who undergo a corneal transplant will need to be monitored closely by their ophthalmologist in the weeks and months following the procedure to ensure that the transplant is successful and to watch for and promptly treat any complications that may arise.
Gregory Scimeca, M.D.
Ophthalmologist and Medical Director
The Eye Professionals
Our Locations
