What is Keratoconus?
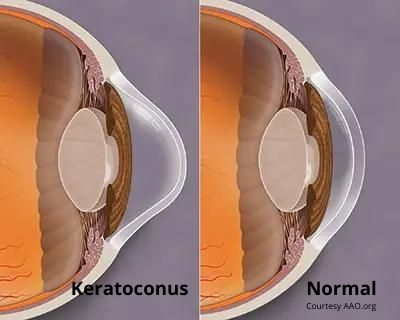
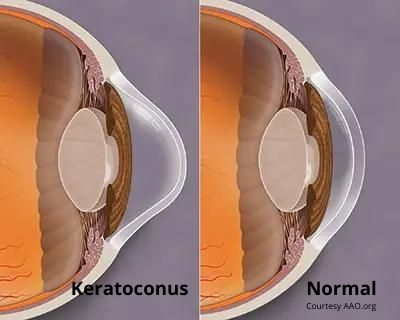
The term means that the cornea is shaped like a cone, and this cone-shaped cornea defect is the most common cornea disorder in the country. Keratoconus, like many medical terms, is a combination of both Latin and Greek. “Keras” means cornea in Greek and “conus” means cone in Latin.
Keratoconus affects one in 2,000 Americans. The condition was first described in medical literature in 1748 and it was first viewed with an ophthalmoscope in 1859. Today keratoconus is well understood by the medical profession, but the cause is not.
Some research suggests that it may be caused by a disruption in the normal levels of enzymes and compounds that control the inflammatory response in the cornea.
This cone-shaped cornea disorder is differentiated into mild, moderate, and advanced conditions. Keratoconus usually develops in a person when they are in their teens or early 20s. It can affect one or both eyes. The condition is progressive, which means the cornea becomes more and more cone-like in shape as time goes on.
Keratoconus causes blurred vision that in the early stage can be corrected with astigmatic glasses, but as the condition progresses, it can get to a point at which the blurry vision cannot be corrected by glasses.
Rigid gas permeable contact lenses help many people with keratoconus by creating an artificial smooth surface on the cornea. Scleral lenses that are wider and fit over both the cornea and the white of the eye can also provide sharper vision for people with keratoconus. Scleral lenses have the added benefit of helping keep the eyes better hydrated than rigid gas permeable lenses.
Medical treatments
Corneal crosslinking (CXL) is a procedure used to strengthen the cornea. The procedure has been used in Europe for more than a decade but was only approved for use in the United States by the FDA in 2016. The procedure uses riboflavin (vitamin B2) eye drops and ultraviolet light to create new collagen crosslinks in the cornea.
The riboflavin eye drops are placed into the eyes over several minutes and then a UV light is directed over the cornea. The interaction between the riboflavin and the UV light causes the formation of reactive oxygen species which then lead to the formation of additional covalent bonds between collagen molecules and this casues the biomechanical stiffening of the cornea.
Stiffening the cornea will slow or prevent the cornea from continuing to thin which causes it to shape itself into a cone.
There are two types of corneal crosslinking procedures. In one the epithelium layer of the cornea is removed before the eye drops and ultraviolet light are used. In the other, the epithelium layer is not removed. This second type is called “epi-on” and is less invasive, takes less time to heal and has less post-procedure complications.
Surgical treatments
About 15-to-20% of keratoconus patients will ultimately require a corneal transplant. Corneal transplants replace the abnormally shaped central portion of the cornea with a donor cornea. The new cornea is held in place with sutures that are removed after healing, which can take from 6-to-18 months.
Corneal transplants result in dramatic improvement in vision for most patients. A cornea transplant removes either the entire thickness or a partial thickness of the diseased cornea and replaces it with a healthy donor cornea.
Corneal transplants are successful for about 90% of the patients who receive them. About 10% of corneal transplants are rejected, but this can often be managed with medications. For patients who do not see well after a corneal transplant, a revision surgery will be used to improve vision.
If you would like to make an appointment, call us 609.877.2800 or EMail us.
Gregory Scimeca, M.D.
Ophthalmologist and Medical Director
The Eye Professionals
Our Locations
